How 3D patient QA highlights uncertainties and catches errors
Carlos Bohorquez, Product Manager for RadCalc and an experienced board-certified clinical physicist speaks about his experiences with 3D secondary checks.
The article was originally published in the Autumn Edition of EMP News by European Federation Of Organizations For Medical Physics – EFOMP.
The field of radiotherapy has been progressing at a tremendous rate over the last couple of decades, leading to more complex treatments with higher doses, sharper gradients, and reduced margins. In turn, a demand has grown within our community for increased guidance of dose metrics for both the efficacy of the treatments and the associated normal tissue complications. (1)(2) Simultaneously, a need to commit to better methods of PSQA has come to light.
Since 2014, I have been investing in this commitment for 3D secondary check systems. As solutions came to market and evolved, many more in our community envisioned the issues that I, too, encountered at the beginning of my journey. Some of these issues, including the increased sensitivity for errors, the need for automation and better efficiency, were highlighted in a great publication (3) that helped me in my first clinical implementation of an independent 3D secondary check.
I have worked with many members in our community as they transition into using 3D secondary checks and have encountered numerous errors in treatment planning. These errors come from a variety of sources and include modeling of delivery systems, such as: MLC leaf ends, MLC tongue‐and‐groove effects, leaf/collimator transmission, collimators/MLC penumbra, compensator systems (scattering, beam hardening, alignment), output factors for small field sizes, head backscatter, and off‐axis profiles. They also include failures in selection of the appropriate dose calculation grid size and the use and modeling of heterogeneity corrections.
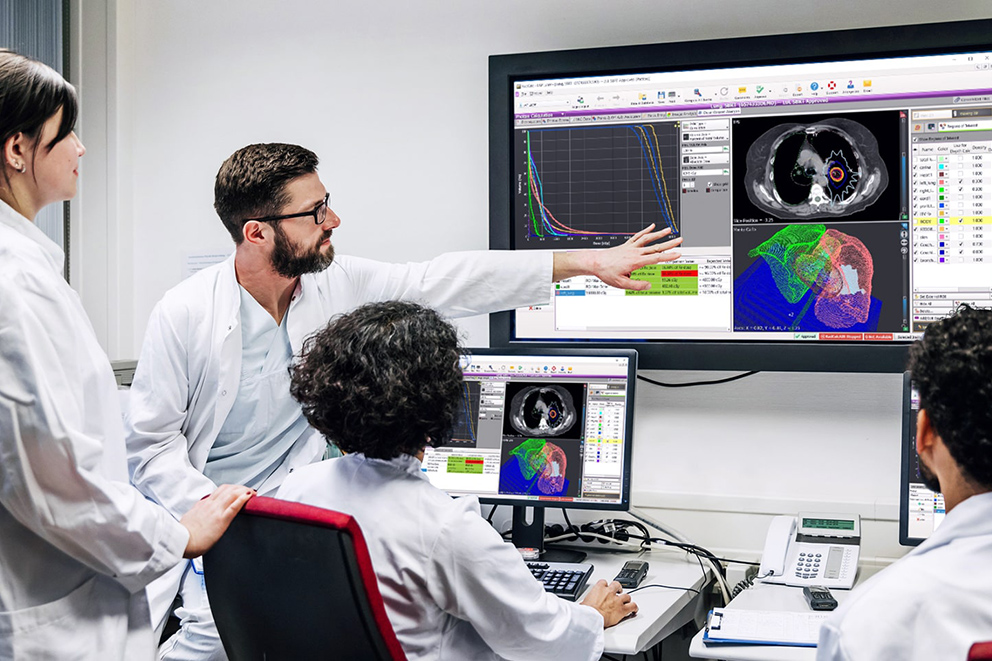
In my experience, 3D secondary checks have caught countless safety issues. However, they tend to also highlight many plan quality issues, like demonstrating differences in doses throughout the whole patient, not just at pre-selected points and 2 dimensional planes. This allows for the evaluation of the dose in every voxel, the ability to do DVH analysis and utilize planning protocols to evaluate specific planning criteria automatically and rapidly.
These observed concerns have now been validated in the release of the AAPM’s Task Group 219 (4), highlighting the limitations of single point comparisons, and recommending a transition to secondary checks that compute the dose distribution of the high dose volume. TG-219 also emphasizes the need for the secondary check to be independent. The report does a great job highlighting the key tasks for acceptance and commissioning of secondary check systems.
Nonetheless, the report misrepresented the commercial solutions available in the market at the time of its publication, mainly that of RadCalc (LifeLine Software, Inc., a part of the LAP Group) and its 3D modules which include both Collapsed Cone Convolution/ Superposition and gold standard Monte Carlo. Released in January of 2020 with version 7.1, RadCalc’s 3D dose modules utilize your clinically measured beam data to bring excellent accuracy. Furthermore, the previously released RadCalcAIR module brings a comprehensive solution to your clinical workflow with intelligent automation features, evolving directly from customer suggestions.
RadCalc 7.1 also offers all the tools needed for a thorough evaluation of treatment plans, such as the ability to separate plans into individual beams and options to automatically add analysis points and lines right from RadCalc, eliminating the need to modify plans within your treatment planning system. RadCalc also places the user in control of their QA program with the flexibility to select the hardware used for the 3D dose calculation and the scalability to fit any clinical network.
Additionally, the AAPM’s Task Group 219, also gives a preview of what’s to come with RadCalc as we integrate the EPID tools from Dosimetry Check (Math Resolutions, LLC) for in air and in vivo dosimetry in our upcoming release!
References:
- Grimm et al. High Dose per Fraction, Hypofractionated Treatment Effects in the Clinic (HyTEC): An Overview. RedJournal 110 (1), May 2021
- Benedict et al. Stereotactic Body Radiation Therapy: The Report of AAPM Task Group 101. Med. Phys. 37 (8), Aug 2010
- Pulliam et al. A six‐year review of more than 13,000 patient‐specific IMRT QA results from 13 different treatment sites. J Appl Clin Med Phys. 2014 Sep; 15(5): 196–206
- Zhu et al. Report of AAPM Task Group 219 on independent calculation- based dose/MU verification for IMRT